Quicklinks
Abdominal & Thoracic Aortic Aneurysm’s
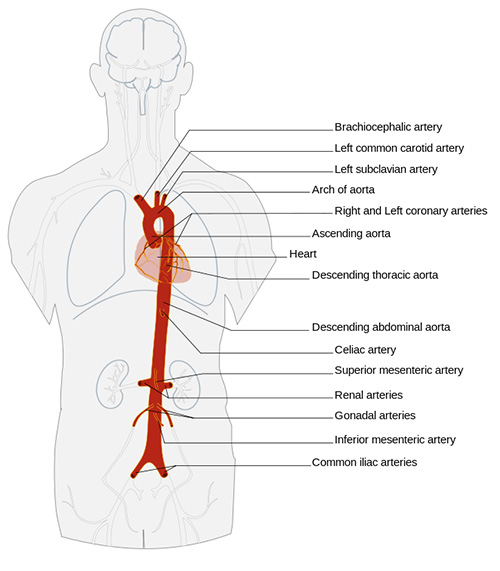
The aorta is the main blood vessel carrying oxygen rich blood from the heart to the rest of the body. The aorta is divided into sections for easy identification. The thoracic aorta is the section located within the chest ending at the diaphragm, and the abdominal section from the diaphragm to approximately the belly button area where the aorta ends and splits in the arteries of the legs.
An aortic aneurysm is a localised ballooning or enlargement of a section of aorta and can occur anywhere along the length of the aorta. Thoracic aneurysms are aneurysms that occur in the chest section of the aorta.
Aneurysms are more common in men than women and in most cases detected in people over 55 years old. Risk factors include a history of smoking, hypertension, high cholesterol, or a known relative with aneurysmal disease. When a person is found to have an aneurysm, their family members should also have screening done after the age of 50 to rule out having an aneurysm.
The majority of aneurysms are stable when detected and only increase in size slowly over several years. Your doctor will monitor the aneurysm by the use of ultrasound and CT scans. Surgical intervention is considered for aortic aneurysms when they reach 5 - 5.5 cms in size, causing abdominal tenderness or showing signs of imminent rupture.

Thoracic Aneurysm

Abdominal Aneurysm
There are two methods of treating an aneurysm when intervention is required.
Open Surgical Repair
An open surgical repair requires a general anaesthesia and the surgeon to make a large incision into your abdomen where the aneurysm is situated. The aneurysmal section of the aorta is then opened and a synthetic tube known as a aortic graft is stitched into place to replace the diseased section. The operation takes about 3-4 hours.
Endovascular Repair
This involves inserting a compressed straight stent (sleeve) or multiple stents (Trouser shaped 2 piece grafts or fenestrated graft) through the femoral arteries in the groin. This can be done by two methods:
Percutaneous method (no surgical exposure of the groin artery) done with a very small incision into the artery with special devices for accessing the artery and closing it on completion of the placement of the stent or small surgical incisions in both groins to expose the femoral arteries. Wires are inserted through the openings into the artery and used to place the synthetic stent in position where it will be expanded to exclude or create a new inner lining of the aorta at the aneurysmal section protecting it from direct contact with high pressure blood flow.
Recovery time is much faster than open surgery with less blood loss, but this type of repair requires ongoing follow up with regular scans to ensure that the graft is working properly. The majority of aneurysm’s are now being repaired by the percutaneous method.
Your Surgeon will discuss with you which type of surgery will suit you.
 Prior to surgery you may need
Prior to surgery you may need
- Blood tests
- CT scan to assess the aneurysm and anatomy for suitability of endovascular repair
- Diagnostic Angiogram
- Cardiology review to assess your heart
- Control of blood pressure
- Antiplatelet therapy
- Respiratory function test
The surgery
- You will be admitted to hospital the day prior to surgery
- You will need to wear ted stocking to help prevent blood clots
- You will spend the first 24 hours in ICU for close monitoring
- You will be given analgesia intravenously or via the epidural catheter
- On discharge to the general ward you will be encouraged to mobilize early to prevent blood clots and lung infections.
- Recovery time is 2-3 days for endovascular repair or 7-10 days for open repair with no complications
Discharge home
- Slowly increase you mobility but no heavy lifting or exercise
- Normal diet
- Take your regular medications
- Change dressings if they become wet and remove after 1 week
- Clinic review in 6-8 weeks and a scan may be required before your visit
- Contact the clinic/GP if you have any fever, rigors, feeling generally unwell, redness, swelling, or discharge from the wound sites
